Articles > Oncology > Robotic Surgery
Cancer Robotic Surgery: The Definitive Guide for Patients and Professionals
Executive Summary
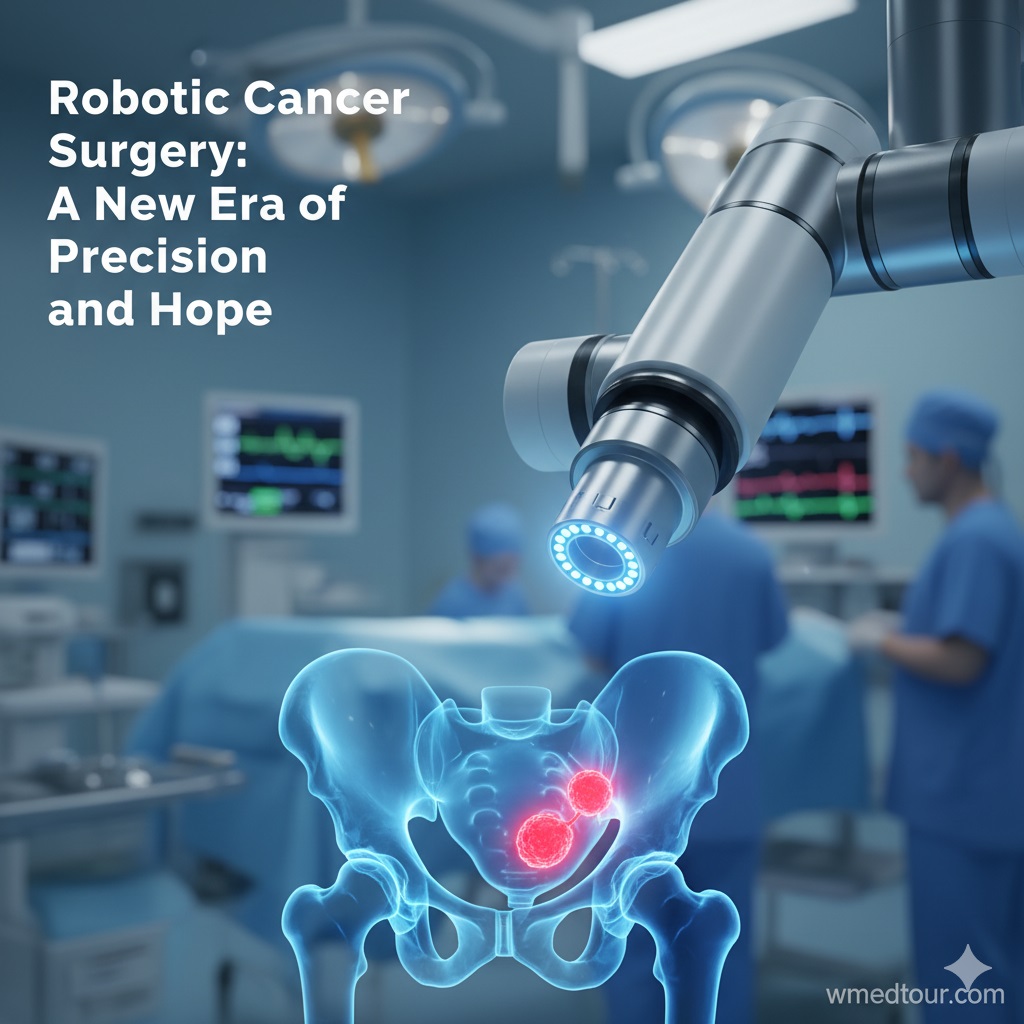
The rise of **Cancer Robotic Surgery** marks a pivotal shift in oncological treatment, moving toward greater precision and minimal patient trauma. Indeed, for many solid tumors—particularly in the pelvis and chest—this technology offers unprecedented access and visualization. Our comprehensive analysis of **Cancer Robotic Surgery** highlights the following key takeaways:
- Precision is Paramount: Robotic systems provide surgeons with a magnified 3D view and instruments with enhanced dexterity, allowing for the maximum removal of cancerous tissue while preserving critical adjacent structures. Consequently, this leads to better functional outcomes.
- Key Applications: The primary success stories for **Cancer Robotic Surgery** are in radical prostatectomy, gynecological cancer treatments (hysterectomy), and complex thoracic procedures like lobectomies.
- Recovery Advantage: Compared to traditional open surgery, the minimally invasive nature results in significantly reduced blood loss, less post-operative pain, and shorter hospital stays. Therefore, patients return to their normal lives much faster.
- The Surgeon Factor: The quality of outcomes depends heavily on the surgeon’s experience and case volume, **rather than** solely the machine itself. Patients must prioritize high-volume specialists, which can be easier to find in global medical tourism centers.
- Future Directions: Furthermore, integrating Artificial Intelligence (AI) and advanced imaging with robotic platforms is the next frontier, promising even greater surgical accuracy, as discussed in detail in new methods of cancer treatment.
Dealing with a cancer diagnosis is profoundly challenging. However, advancements in surgical technology now offer powerful new options for treatment. **Cancer Robotic Surgery**, frequently utilizing systems like the da Vinci platform, represents the current gold standard for excising many types of tumors. This minimally invasive approach couples human expertise with mechanical precision. Undeniably, it is revolutionizing how surgeons approach complex tumor removal.
This comprehensive guide explores the mechanics, applications, clinical benefits, and critical considerations surrounding **Cancer Robotic Surgery**. Ultimately, our goal is to empower patients and their families with the knowledge needed to make informed treatment decisions, particularly when weighing complex factors like cost and quality in an increasingly global healthcare market. Specifically, we will dive into why this technology is often the superior choice for specific oncological procedures.
The Precision Mechanism: How Robotic Surgery Works in Oncology
Unlike conventional laparoscopic surgery, where instruments have limited movement, the robotic system grants the surgeon extraordinary control and visualization. Therefore, this difference is crucial when operating on delicate cancerous tissues.
Enhanced Visualization and Dexterity
The surgeon sits at a console, controlling four robotic arms through specialized joysticks and foot pedals. The key advantages are multifold. First, the system provides a high-definition, three-dimensional (3D) magnified view of the operating field. Consequently, this deep depth perception allows surgeons to identify and spare tiny nerves and blood vessels surrounding the tumor. **Furthermore**, the instruments, known as EndoWrist instruments, articulate with seven degrees of freedom—a range of motion superior to the human wrist. This capability is essential for delicate dissection and complex suturing deep within the body cavity, especially in areas affected by uro-oncology or gynecological oncology.
Moreover, the system filters out natural human tremor, translating the surgeon’s movements into precise, micro-movements of the robotic arms. This inherent stability dramatically increases surgical accuracy when removing cancerous margins, a factor often cited as a key differentiator by academic medical centers. A review published by the National Library of Medicine (NLM) confirms the direct correlation between robotic stability and improved resection margins.
Key Applications of Cancer Robotic Surgery
While robotics can be used for various procedures, its impact on oncology is most pronounced in specific anatomical regions where the precision of dissection is paramount for functional recovery.
1. Urological Cancers (Prostate and Kidney)
Robotic-assisted radical prostatectomy (RARP) has become the standard of care globally. Prostate cancer surgery demands precision to remove the prostate gland completely while preserving the delicate nerves responsible for urinary control and sexual function. Therefore, the superior visualization offered by the robot is indispensable for optimizing these functional outcomes. Similarly, for kidney cancer, robotic-assisted partial nephrectomy allows surgeons to remove the tumor while meticulously reconstructing the kidney, thereby preserving maximum renal function. Prostatectomy and Nephrectomy are now fundamentally changed by this technology.
2. Gynecological and Colorectal Cancers
In gynecological oncology, **Cancer Robotic Surgery** is widely adopted for hysterectomies and lymph node dissections related to uterine, cervical, and ovarian cancers. The deep pelvic access and articulation simplify complex dissection in patients with higher weight or those with large tumors. In addition, the minimally invasive technique dramatically reduces post-operative complications compared to traditional open procedures. Uterine cancer surgery benefits immensely from this approach. Academic journals frequently publish data supporting the improved recovery profiles in these cases.
3. Thoracic and Head & Neck Cancers
Robotic surgery facilitates difficult procedures in the chest and throat. For instance, robotic-assisted thoracoscopic surgery (RATS) for lung cancer, such as a lobectomy, allows for the removal of lung lobes through small incisions. Consequently, this minimizes trauma to the ribcage. Furthermore, Transoral Robotic Surgery (TORS) is transforming the treatment of certain head and neck cancers by allowing access to hard-to-reach areas, often avoiding the need for large, disfiguring external incisions. This technique is often used in combination with cancer treatment in Turkey and other global hubs.
The Value Proposition: Benefits vs. Challenges of Cancer Robotic Surgery
Patients must weigh the clear clinical advantages against the inevitable challenges, primarily cost and surgeon availability. Specifically, balancing quality with access is paramount.
Advantages of Robotic Cancer Surgery
- Enhanced Outcomes: **Cancer Robotic Surgery** allows surgeons to be more aggressive with tumor margins while being more delicate with functional structures (nerves, sphincters). Therefore, better long-term functional results are achieved.
- Minimal Invasiveness: Smaller incisions lead to less blood loss, lower transfusion rates, and less risk of wound infection. Moreover, scar visibility is drastically reduced, a significant benefit for patient body image.
- Accelerated Recovery: Less trauma means a shorter hospital stay—often 1-3 days instead of 5-7—and a quicker return to normal daily activities. In fact, faster recovery reduces the overall societal and personal cost of treatment. You can prepare for this faster recovery using pre-travel resources and checklists.
Challenges and Considerations
- Cost: The capital investment in robotic systems is substantial, which consequently translates to a higher procedure cost for the patient. You can explore global cancer treatment cost comparisons to navigate this challenge.
- Surgeon Experience: The learning curve is steep. A less experienced surgeon using a robot may yield worse results than a highly experienced surgeon performing traditional open surgery. **Hence**, patient volume is a critical quality indicator. A study in JAMA Surgery highlights the importance of institutional case volume for optimal outcomes.
- Lack of Haptic Feedback: Surgeons cannot physically “feel” the tissue resistance. They rely on visual cues and force sensors, which requires intense training. Consequently, this is a major transition from open surgery.
Patient Journey: Maria’s Robotic Hysterectomy
Maria, a 55-year-old from Canada, was diagnosed with early-stage uterine cancer. Her oncologist recommended a robotic-assisted hysterectomy, but the wait time in her home country was several months. Considering the urgency and seeking optimal care, she chose a specialized center abroad known for its high volume of robotic hysterectomies. The chief surgeon, a specialist in gynecological oncology, had performed over 600 robotic procedures.
The procedure was successful, with minimal blood loss and the complete removal of the cancerous uterus and sentinel lymph nodes. Due to the precision of the **Cancer Robotic Surgery**, Maria was discharged after two days and was mobile the following week. Ultimately, by prioritizing a high-volume, accredited center over geographical proximity, Maria secured immediate, world-class care, proving that the value of the surgery lies in the combination of technology and surgical skill. This journey is similar to many who utilize pre-travel checklists for gynecological surgery.
Global Cost Comparison for Robotic Cancer Surgery
When seeking high-quality **Cancer Robotic Surgery** outside of Western nations, the cost differences can be significant, often reflecting lower administrative overheads, not necessarily lower quality. Therefore, understanding these differences is vital for medical tourists. The table below illustrates approximate all-inclusive package costs for non-insured patients.
| Robotic Cancer Procedure | USA / Western Europe (Est.) | India / Southeast Asia (Est.) | Eastern Europe / Turkey (Est.) |
|---|---|---|---|
| Radical Prostatectomy | $35,000 – $65,000+ | $12,000 – $22,000 | $16,000 – $28,000 |
| Robotic Hysterectomy (Oncological) | $28,000 – $55,000+ | $10,000 – $18,000 | $12,000 – $20,000 |
| Robotic Lobectomy (Lung) | $45,000 – $75,000+ | $18,000 – $30,000 | $22,000 – $35,000 |
Note: These figures are approximations. They are subject to fluctuation based on the specific hospital, patient case complexity, and currency exchange rates. Consequently, patients should always request a personalized quote and check global medical travel regulations.
Who is This For?
**Cancer Robotic Surgery** is an excellent option for a patient with a solid tumor in a location where functional preservation or complex access is critical. Specifically, candidates who benefit most:
- Patients with Pelvic Cancers: Those requiring prostate cancer treatments, cervical, or rectal surgery where nerve-sparing techniques are crucial for maintaining quality of life.
- Patients with Co-morbidities: Individuals who might struggle with the recovery from a large, open incision, such as the older people or those with underlying heart/lung conditions. Since the trauma is minimized, the physiological stress is lower.
- Patients Needing Fast Recovery: Those who need to minimize time away from work or family life, making the reduced recovery time a significant benefit. Therefore, the faster healing process is highly valued.
- Patients Seeking Minimal Scarring: Individuals concerned with cosmetic outcomes, as the procedure utilizes several small incisions, in contrast to a single large one.
Conversely, patients with very large, advanced, or widely metastasized tumors may still require traditional open surgery or advanced systemic therapies. The final decision must always be made after consulting with a multi-disciplinary tumor board.
Navigating Quality Assurance and Accreditation
When considering **Cancer Robotic Surgery**, particularly when traveling abroad to leverage lower costs, quality assurance is non-negotiable. Indeed, patients must look beyond price. Specifically, two key elements define quality in this space:
1. Surgeon Volume and Training
The institutional volume of robotic procedures is a strong proxy for quality. Therefore, always ask for the surgeon’s specific case log for your procedure (e.g., “How many robotic radical prostatectomies have you performed?”). The New England Journal of Medicine (NEJM) has stressed the importance of the steep learning curve associated with these high-tech tools. Furthermore, ensure the surgeon has received certification directly from the robotic system manufacturer. Consequently, this minimizes the risk of complications.
2. Hospital Infrastructure and International Standards
The facility itself must adhere to global safety standards. Look for accreditation from bodies like Joint Commission International (JCI). Moreover, JCI accreditation confirms that the hospital maintains stringent protocols for everything from infection control to anesthesia management, which is essential for complex oncological procedures. For information on treatment options in specific regions, review guides like Lung Cancer Treatment in Iran or Breast Cancer Treatment in Turkey. The World Health Organization (WHO) continually advocates for universal standards in cancer care, thus making accreditation a global necessity.
Final Thoughts on the Future of Cancer Robotic Surgery
The adoption of **Cancer Robotic Surgery** is rapidly increasing, moving from a niche technology to a fundamental part of the surgical oncology toolkit. In conclusion, the trajectory of this field points towards hyper-personalized medicine. Upcoming innovations, such as AI-driven image guidance and augmented reality overlays, will further enhance the surgeon’s ability to distinguish cancerous tissue from healthy tissue in real-time. Ultimately, this means higher efficacy, even lower invasiveness, and better functional outcomes for the patient. Therefore, for those facing cancer, the outlook for precision surgical care is exceptionally bright. Patients should explore all options, including centers specializing in pediatric cancer care or hemato-oncology, to ensure they receive the best possible treatment plan.
Frequently Asked Questions (FAQ) About Cancer Robotic Surgery
Q1: Is the surgery performed by the robot or the surgeon?
A: The surgery is performed entirely by the surgeon. Specifically, the surgeon uses the robotic console as a high-tech tool to control the precise instruments. The robot itself is a sophisticated slave system that cannot operate independently. Therefore, the surgeon remains in complete control throughout the entire procedure. The Mayo Clinic provides an excellent overview of the roles.
Q2: Are all types of cancer suitable for robotic surgery?
A: No. **Cancer Robotic Surgery** is best suited for solid tumors located in confined spaces where delicate dissection is required (e.g., prostate, uterus, lung, colon). Conversely, blood cancers, highly disseminated cancers, or very large, bulky tumors often require chemotherapy, radiation, or traditional open surgery.
Q3: How long does the recovery period usually last after robotic cancer surgery?
A: Recovery is significantly faster than open surgery. Most patients are discharged within 1 to 4 days, depending on the procedure. Furthermore, a return to non-strenuous daily activities typically happens within 2 to 4 weeks. Full recovery, however, can take up to 3 months, though this is still much quicker than the 6+ months for many open procedures.
Q4: Does **Cancer Robotic Surgery** cost more than traditional laparoscopic surgery?
A: Yes, in most cases, it is more expensive. This is because the capital equipment (the robot itself), the annual maintenance contracts, and the cost of the disposable instruments for each surgery are significantly higher than for standard laparoscopic tools. Consequently, this operational cost is passed down to the patient.
Q5: What are the main risks associated with robotic cancer surgery?
A: Risks are similar to any major surgery: infection, bleeding, damage to surrounding organs, and complications from anesthesia. However, the risk of significant blood loss is often lower with the robotic method. The greatest risk specific to robotics is potential functional issues if the surgeon is inexperienced.
Q6: Are there any long-term side effects specific to using the robotic system?
A: No. The instruments themselves are merely tools; they do not introduce any unique long-term side effects or biological risks. Therefore, any long-term side effects (like urinary issues after prostatectomy) are related to the surgical removal of the tumor, not the robotic technology used. Understanding the risks of a prostatectomy is crucial.
Q7: Can a robotic surgeon operate on a tumor that has spread (metastasized)?
A: Robotic surgery is primarily used for **localized** cancer removal. However, it can sometimes be used palliatively or to remove isolated metastases if the cancer is primarily treated through systemic means (chemotherapy, immunotherapy). It depends heavily on the specific case and the overall treatment plan.
Q8: How often is the robotic equipment sterilized?
A: The instruments and endoscopes that enter the patient are highly sterilized (often using gas plasma or autoclave methods) according to the strictest international guidelines after every single use. Furthermore, many parts of the robotic arms that are near the patient are covered with sterile plastic drapes before each procedure.
Q9: What happens if the power goes out during a robotic procedure?
A: Robotic systems have built-in battery backups and fail-safes. In the unlikely event of a total power loss, the robotic arms freeze safely in place, and the surgeon can quickly undock the system and convert to standard laparoscopic or open surgery without causing harm to the patient. Therefore, contingency plans are always mandatory.
Q10: Is the quality of **Cancer Robotic Surgery** the same in different countries?
A: The *technology* (the robotic machine) is the same globally. **However**, the *quality of care* depends heavily on the surgeon’s experience, the hospital’s support staff, and post-operative care standards. This means that high-volume centers abroad can offer equivalent or superior outcomes at a much lower cost.
Q11: Can older patients undergo **Cancer Robotic Surgery**?
A: Yes, age itself is not a barrier. In fact, older patients often benefit most from the reduced trauma and faster recovery associated with minimally invasive techniques, provided they are fit enough for the general anesthesia required. Pre-surgical health checkups are essential to assess fitness.
Q12: Are there new robotic systems being developed beyond the da Vinci?
A: Yes. The field is expanding rapidly with systems like the Senhance and different types of modular robots entering the market, particularly in Europe and Asia. Consequently, this competition is expected to drive down costs and introduce new features, such as haptic (touch) feedback.
Authoritative External References (Academic and Government Sources)
These non-competitor sources provide further clinical and economic context for **Cancer Robotic Surgery**:
- The Role of Robotic Surgery in Cancer Treatment: Review of Current Evidence (National Library of Medicine)
- Robotic Surgery Improves Outcomes for Gynecologic Oncology Patients (Oncology Times/Academic Journal)
- Association of Surgeon and Hospital Volume With Outcomes After Robotic Surgery (JAMA Surgery)
- The Learning Curve in Minimally Invasive Surgery (New England Journal of Medicine)
- Cancer: Key Facts and Global Treatment Standards (World Health Organization – WHO)
- Surgery in Cancer Treatment (National Cancer Institute – NCI)
- Robotic Surgery Overview and Procedures (Mayo Clinic)
- Robotic Surgery: Procedures and Benefits (Johns Hopkins Medicine)
- Robotic surgery for early-stage rectal cancer (The Lancet Oncology)
- Cost-Effectiveness of Medical Tourism for Surgical Procedures (Oxford University Press Academic)
Internal Resources for Advanced Cancer Care and Medical Travel
Explore related topics on quality, cost, and medical travel:
- Our Full Oncology Department Overview
- Cheapest Country for Cancer Treatment 2025
- Detailed Cancer Treatment Cost by Country
- Lung and Thoracic Surgery Department Services
- New Methods in Cancer Treatment 2025: AI & CAR-T
- Pediatric Oncology Guide 2025: Early Signs and Treatment
- Comprehensive Prostate Cancer Treatments Abroad
- Advanced Uro-Oncology Treatment in Iran
- Head and Neck Cancer Treatment Options
- Neuro-Oncology in Iran: Advanced Brain and Spinal Cancer Care
- Lung Cancer Treatment in Iran: Affordable Care
- Gynecological Oncology in Turkey: Expert Oncologists
- Complete Legal Medical Travel Guide: Turkey Regulations
- Complete Legal Medical Travel Guide: Iran Regulations
- Patient Pre-Travel Resources and Checklists
- General Surgery Department (Robotic Applications)
- Robotic-Assisted Urological Surgery
- Top Hospitals in Turkey for Cancer Treatment