⚕️ Bone Marrow Transplant: A Comprehensive Guide to the Procedure, Types, and Recovery
Authored by Wmedtour Experts | Visit us at https://www.wmedtour.com
📋 Executive Summary
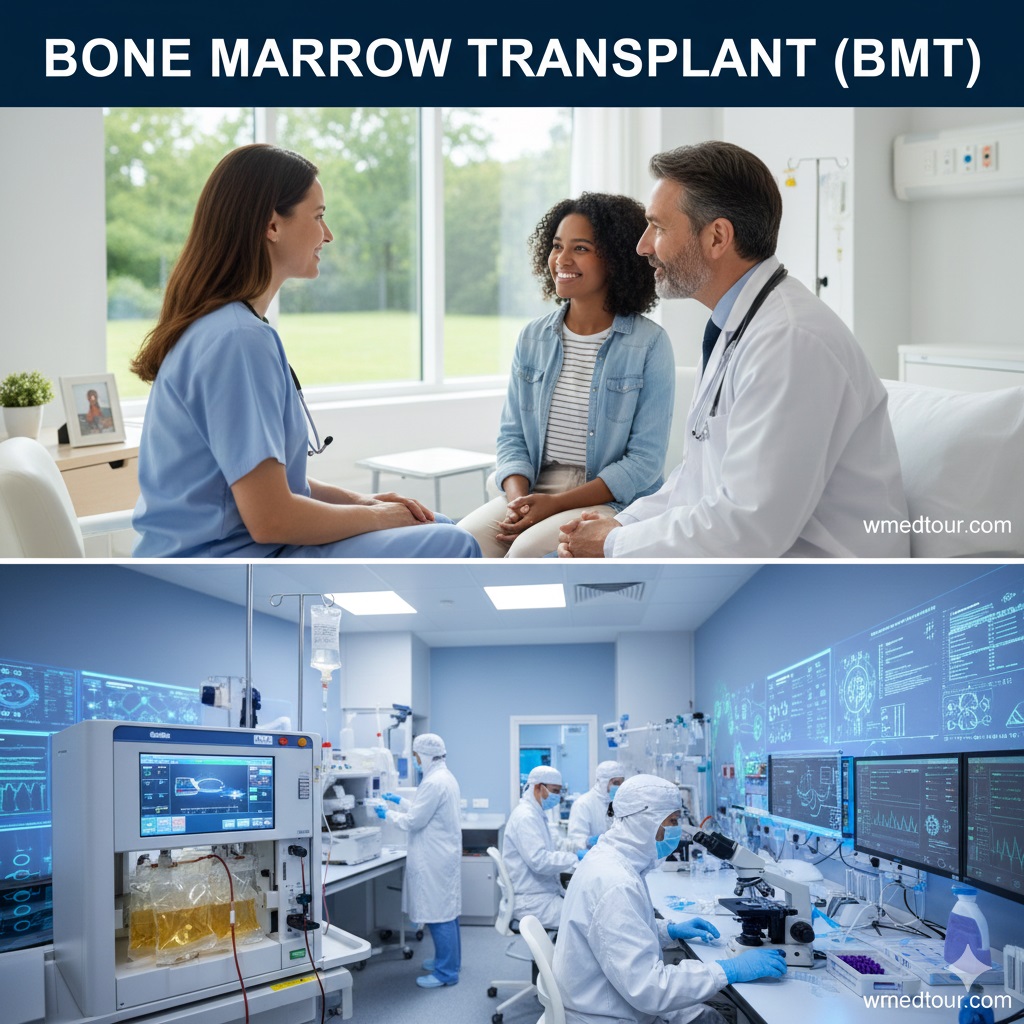
A bone marrow transplant (BMT)—also known as a Hematopoietic Stem Cell Transplant (HSCT)—represents a complex, life-saving medical procedure. Therefore, understanding its intricacies is absolutely vital for patients and their families. This treatment involves replacing damaged or diseased bone marrow with healthy blood-forming stem cells. Consequently, this process restores the body’s ability to produce functional blood components. This guide systematically breaks down the entire process, differentiating between the two primary methods—autologous (using the patient’s own cells) and allogeneic (using a donor’s cells). We detail the intensive conditioning regimen, the infusion process, the challenging recovery period, and the long-term outlook. Furthermore, we clarify the essential concepts of Human Leukocyte Antigen (HLA) matching and the critical complication of Graft-versus-Host Disease (GVHD), providing an authoritative, yet easy-to-understand overview for everyone.
🧬 What Exactly is a Bone Marrow Transplant (BMT)?
The term bone marrow transplant (BMT) refers to a procedure that infuses healthy blood-forming stem cells into a patient’s body. Primarily, the goal is to rescue the patient’s system after high doses of chemotherapy or radiation have destroyed their diseased bone marrow. Consequently, this high-dose therapy eliminates the diseased cells. The core of this treatment relies entirely on hematopoietic stem cells (HSCs), which are the progenitor cells for all blood components: red blood cells, white blood cells, and platelets. [Image of Bone Marrow and Hematopoietic Stem Cells]
🔬 The Vital Role of Stem Cells
Stem cells are uniquely capable of self-renewal and differentiating into various specialized cell types. However, when diseases like leukemia, aplastic anemia, or immune deficiency syndromes strike, the bone marrow—the soft, spongy tissue inside your bones—fails to function correctly. Therefore, a bone marrow transplant becomes the definitive treatment option. This intervention fundamentally resets the body’s entire blood-producing factory. Preimplantation Genetic Testing, while usually related to fertility, highlights the intense cellular level at which modern medicine operates, similar to the cellular focus of BMT.
Indeed, this process is far more involved than a simple blood transfusion. Furthermore, it represents a complete replacement of the patient’s immune and hematologic system. Consequently, the patient must undergo rigorous preparation and face a prolonged, complex recovery period. Because of these challenges, it necessitates comprehensive and highly specialized medical care.
🎯 Why Do Doctors Perform a BMT? (Key Indications)
A bone marrow transplant serves several critical medical purposes, primarily addressing conditions where the bone marrow is malfunctioning or needs replenishment after intense therapy. Importantly, the main diseases treated fall into three categories.
Malignant (Cancerous) Conditions:
Chiefly, BMT treats blood cancers. This includes various forms of leukemia (Acute Myeloid Leukemia – AML, Acute Lymphoblastic Leukemia – ALL, Chronic Myeloid Leukemia – CML), lymphomas (Hodgkin and non-Hodgkin), and multiple myeloma. In these cases, the high-dose chemotherapy aims to eliminate every cancerous cell, and the transplant subsequently restores the patient’s destroyed blood system. For solid tumors, such as high-risk pediatric neuroblastoma, BMT is sometimes used as a rescue measure following aggressive treatment, much like other specialized cancer treatments such as CAR T-cell therapy for pediatric neuroblastoma.
Non-Malignant Conditions:
Additionally, BMT can correct non-cancerous diseases that result from genetic defects or bone marrow failure. These disorders include severe aplastic anemia, Fanconi anemia, and various hemoglobinopathies such as sickle cell disease and thalassemia. Moreover, BMT is indispensable for certain inherited immune deficiencies, like Severe Combined Immunodeficiency (SCID), often referred to as “bubble boy disease,” allowing the patient to develop a fully functional immune system.
🔄 The Different Types of Bone Marrow Transplant
Specialists classify bone marrow transplant procedures based on the source of the donated stem cells. This distinction is paramount because it dictates the potential complications, donor selection, and overall treatment strategy.
🤝 Allogeneic Transplant (Allo-BMT): The Donor Approach
The allogeneic method involves receiving stem cells from a donor. This donor may be related (a sibling or parent) or unrelated (found through a national or international registry, like the global efforts to find donors for kidney donation in legal countries). Significantly, the success of this type of BMT hinges on Human Leukocyte Antigen (HLA) matching.
Donor Sources for Allo-BMT:
There are several potential sources for allogeneic stem cells. Most commonly, a matched sibling is the best option. However, if a match is unavailable, doctors search international registries for a matched unrelated donor (MUD). Furthermore, two other crucial options exist: cord blood (blood collected from the umbilical cord after birth) and haploidentical donation, which uses a half-matched donor, typically a parent or child. Furthermore, the haploidentical approach has become increasingly common in recent years due to improved immunosuppression protocols.
Pros and Cons of Allogeneic BMT
Pros: The primary advantage is the “graft-versus-leukemia” (GVL) effect. This occurs because the donor’s immune cells recognize any residual cancer cells in the recipient as foreign and attack them, providing an ongoing cancer-fighting benefit. This is a powerful, long-term anti-cancer mechanism.
Cons: Conversely, the biggest risk is Graft-versus-Host Disease (GVHD). This condition occurs when the donated immune cells attack the recipient’s healthy tissues, often leading to severe, chronic issues affecting the skin, liver, and gut. Another risk is graft failure, where the donor cells do not engraft or are rejected.
👤 Autologous Transplant (Auto-BMT): The Self-Rescue
An autologous bone marrow transplant uses the patient’s own stem cells. In this procedure, doctors collect the patient’s healthy stem cells, usually from their peripheral blood, and freeze them. Subsequently, the patient undergoes high-dose chemotherapy or radiation to kill the cancer cells. Immediately following this intense treatment, the stored cells are thawed and infused back into the patient’s bloodstream, rescuing their bone marrow function. This method is frequently used for diseases like multiple myeloma and non-Hodgkin lymphoma.
Pros and Cons of Autologous BMT
Pros: The foremost benefit is the complete absence of GVHD and transplant rejection, as the patient receives their own cells. Consequently, this leads to faster immune recovery and a shorter hospital stay compared to allo-BMT. The procedure is generally safer in the short term.
Cons: Nevertheless, a significant drawback is the lack of the GVL effect, meaning the patient relies solely on the chemotherapy to eradicate the cancer. Furthermore, there is a small risk that cancerous cells might have been collected and stored along with the healthy stem cells, potentially leading to relapse. This risk requires careful cell processing before freezing.
🗺️ The Bone Marrow Transplant Journey: Step-by-Step
The path to a successful bone marrow transplant is demanding and structured, typically unfolding over several phases, each with its unique challenges and protocols.
1️⃣ Step 1: Pre-Transplant Workup and Conditioning
The workup phase ensures the patient is physically fit enough to endure the BMT process. Doctors perform thorough heart, lung, and organ function tests. Once cleared, the patient enters the conditioning phase.
The Conditioning Regimen: Clearing the Way
This critical phase involves giving high-dose chemotherapy, sometimes combined with total body irradiation (TBI). The primary goal is twofold: eradicate all remaining cancer cells and suppress the patient’s immune system to prevent it from rejecting the new graft (in allo-BMT). Doctors classify regimens based on intensity:
- Myeloablative Conditioning (MAC): This is the traditional, high-intensity regimen that completely destroys the patient’s bone marrow.
- Reduced-Intensity Conditioning (RIC) or “Mini-Transplant”: This less aggressive approach uses lower doses of chemotherapy, relying more heavily on the GVL effect from the donor cells to eliminate cancer. RIC is often preferred for older or frailer patients.
Pros of MAC: Higher chance of cancer eradication upfront. Cons of MAC: Significantly higher toxicity and risk of long-term organ damage.
Pros of RIC: Lower initial toxicity, broader eligibility for BMT. Cons of RIC: Higher risk of graft failure or early relapse compared to MAC.
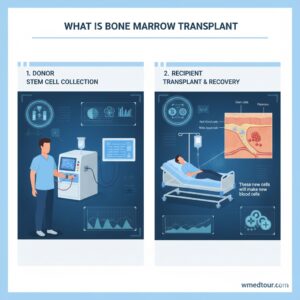
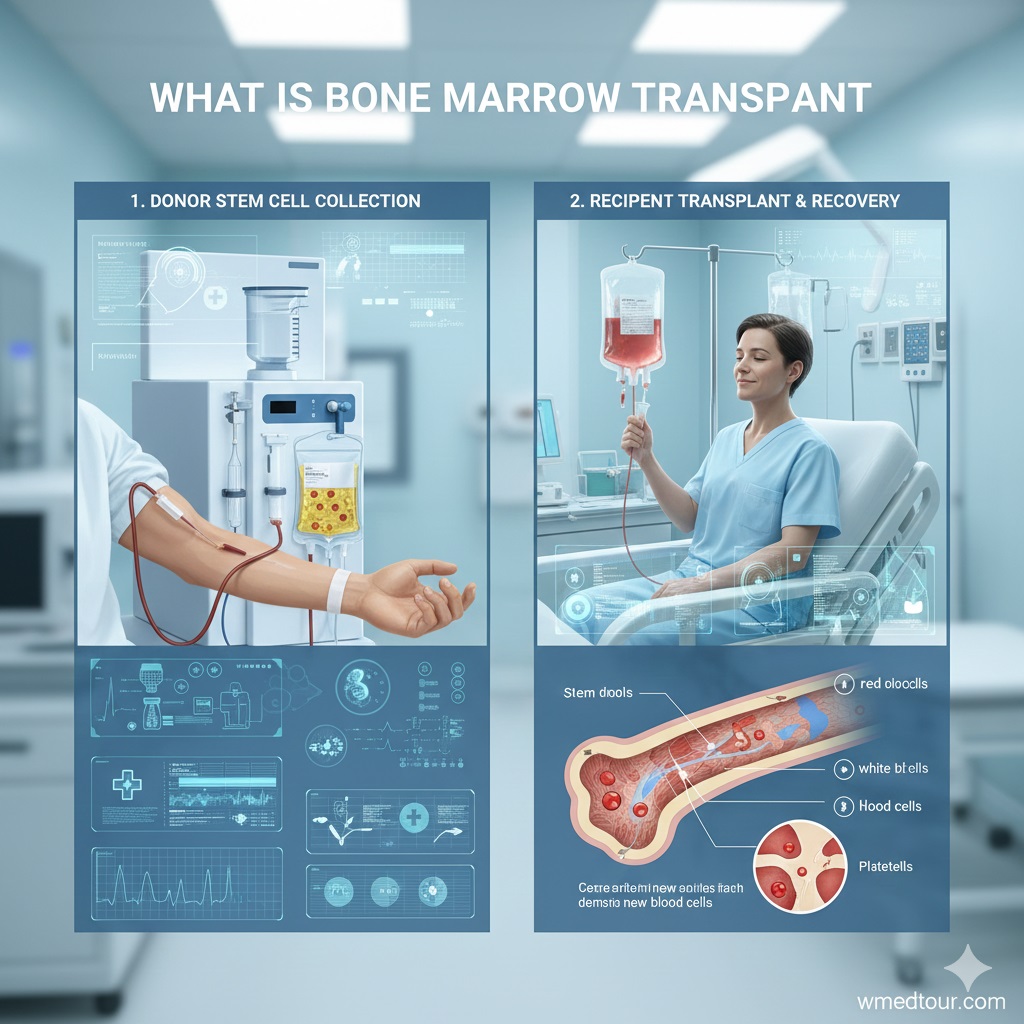
2️⃣ Step 2: Stem Cell Infusion (Transplant Day)
The day of the infusion is remarkably anti-climactic. The healthy stem cells, collected from the donor or previously stored from the patient, are infused intravenously, much like a simple blood transfusion. The cells travel through the bloodstream, finding their way to the bone marrow spaces—a biological process known as “homing.” Furthermore, the patient is awake during the procedure, which is generally painless. Nevertheless, some patients might experience minor side effects like fever or chills due to the preservative used during freezing.
This step marks the beginning of the crucial post-transplant period, sometimes involving specialized care that echoes the complexity found in procedures like cardiac surgery involving EPS RFA ablation.
3️⃣ Step 3: Engraftment and Early Recovery
Following the infusion, the patient enters the most high-risk period, generally lasting three to four weeks. Importantly, the patient’s blood counts drop critically because the conditioning regimen destroyed the original marrow.
The Period of Neutropenia:
During this time, known as neutropenia, the patient possesses virtually no immune system, making them extremely susceptible to infection. Therefore, they must remain in protective isolation. However, doctors administer countless blood transfusions and powerful intravenous antibiotics to support them through this vulnerable stage. Subsequently, engraftment occurs when the new stem cells begin producing white blood cells, typically signaled by a rising neutrophil count. Securing a medical visa for such a long hospitalization is often a crucial logistical step for international patients.
✅ Who is This For?
The determination of whether a bone marrow transplant is appropriate involves a highly specialized risk-benefit assessment. Indeed, BMT is a treatment reserved for patients facing life-threatening hematologic diseases or cancers where standard chemotherapy alone is insufficient for cure.
This procedure is generally for individuals who meet specific criteria. Firstly, they must have a diagnosis proven to respond to BMT, such as high-risk acute leukemia, refractory lymphoma, or severe bone marrow failure. Secondly, the patient must be medically fit enough to withstand the intense conditioning and recovery phases, meaning they should have adequate heart, lung, liver, and kidney function. Since BMT profoundly affects the immune system, it is often considered a last-resort or definitive curative option. For patients considering complex procedures globally, understanding the process is as vital as researching options like the best country for open heart surgery.
⚠️ Breakdown of Risks and Complications in BMT
Although a bone marrow transplant offers curative potential, it carries significant, potentially life-threatening risks. Consequently, comprehensive patient counseling is essential.
💥 Allogeneic-Specific Complication: Graft-versus-Host Disease (GVHD)
GVHD is the most unique and devastating risk of allogeneic BMT. The new immune system, derived from the donor, recognizes the recipient’s healthy cells as foreign and launches an attack. This is a complex immunological problem.
Acute vs. Chronic GVHD
Acute GVHD: This typically occurs within the first 100 days post-transplant, affecting the skin (rash), liver (jaundice), and gastrointestinal tract (diarrhea/cramps).
Chronic GVHD: This is a more complex, long-term condition that can mimic autoimmune diseases. It can affect almost any organ, including the eyes, mouth, lungs, and joints, requiring years of careful immunosuppressive therapy. Furthermore, managing chronic GVHD significantly impacts the patient’s quality of life.
GVHD Pros and Cons (The Double-Edged Sword)
Pros (The Paradox): A mild form of GVHD often correlates with a stronger GVL effect, meaning a lower chance of cancer relapse. Therefore, doctors sometimes view a touch of GVHD as a sign that the donor cells are active.
Cons: Severe, life-threatening GVHD can cause irreversible organ damage, often requiring intense, prolonged treatment that itself carries risks like infection.
🦠 Risks Common to Both Allo- and Auto-BMT
Both transplant types share several risks stemming primarily from the intense conditioning regimen.
Infection Risk:
The period of neutropenia exposes patients to bacterial, fungal, and viral infections. This risk persists for many months until the new immune system fully develops. Global medical treatment regulations mandate strict hygiene protocols during this recovery phase.
Organ Toxicity and Damage:
High-dose chemotherapy and radiation can cause significant, permanent damage to organs such as the heart, lungs, liver, and kidneys. Consequently, Veno-Occlusive Disease (VOD) of the liver is a particularly severe complication.
Relapse:
Ultimately, the cancer can return. Relapse remains the most common cause of death following BMT, especially if the disease was advanced before the procedure. Considering cancer treatment cost by country highlights the financial burden of managing relapse.
🔍 The Crucial Role of Donor Matching (HLA Typing)
For an allogeneic bone marrow transplant, finding the perfect match is absolutely non-negotiable. This matching relies on Human Leukocyte Antigens (HLA), which are markers on the surface of most cells. HLA genes reside on chromosome 6, and matching these markers minimizes the risk of the recipient rejecting the donor cells (graft failure) or the donor cells attacking the recipient (GVHD). Generally, doctors test for 10 or 12 key HLA markers, aiming for the highest possible score.
📊 Comparison Table: Allogeneic vs. Autologous BMT
To clarify the distinction, here is a concise comparison of the key aspects of the two main types of bone marrow transplant.
| Feature | Allogeneic Transplant (Allo-BMT) | Autologous Transplant (Auto-BMT) |
|---|---|---|
| Stem Cell Source | Matched related or unrelated donor. | Patient’s own previously collected cells. |
| Need for HLA Match | Absolutely essential (higher match = lower risk). | Not applicable. |
| Graft-versus-Host Disease (GVHD) | Primary risk, ranging from mild to life-threatening. | Zero risk. |
| Graft-versus-Tumor (GVT) Effect | Present and desired; provides immune surveillance against cancer. | Not present. |
| Primary Indication Example | High-risk acute leukemias, severe aplastic anemia. | Multiple myeloma, relapsed Hodgkin’s lymphoma. |
| Recovery Timeline | Slower immune recovery (6-12+ months). | Faster immune recovery (3-6 months). |
📘 Patient Journey: A Hypothetical Case Study
Consider the case of Elias, a 45-year-old patient diagnosed with high-risk Myelodysplastic Syndrome (MDS) that progressed to Acute Myeloid Leukemia (AML). Because his chemotherapy failed to achieve long-term remission, an allogeneic bone marrow transplant was his only curative option.
The Road to Transplant
Firstly, a search was initiated, and fortunately, a fully matched unrelated donor (MUD) was identified through a registry. Subsequently, Elias underwent a thorough physical assessment, including comprehensive health checkups to ensure his organs could withstand the procedure. On Day -7, his conditioning regimen—a high-dose combination of busulfan and cyclophosphamide (MAC)—began. This intensive treatment left him extremely fatigued and immunosuppressed, completely destroying his cancerous marrow.
Infusion and Engraftment
On Day 0, Elias received the donor cells, infused slowly via his central venous catheter. Following this, he entered the critical neutropenic phase. He was hospitalized for five weeks, during which he battled a fungal infection due to his lack of white blood cells. Finally, on Day +18, his doctors confirmed engraftment; his neutrophil count rose above the critical threshold, marking the beginning of his new immune system’s functionality.
Post-BMT Challenges
Unfortunately, Elias developed mild acute GVHD affecting his skin (a subtle rash), which was managed with low-dose steroids. Six months later, he successfully transitioned to the outpatient clinic. Importantly, while his recovery was long—a full year before he felt truly back to normal—the transplant achieved its goal: he remains in complete remission, benefiting from the donor’s immune system constantly surveying for any signs of relapse. His journey underscores the necessity of having robust medical and logistical support, much like patients planning for medical travel to Iran need detailed preparation.
🌱 Post-Transplant Life and Long-Term Outlook
The period immediately following discharge, often known as the post-transplant period, is characterized by ongoing vigilance and slow rebuilding. It is a marathon, not a sprint.
The Long Road to Immunological Recovery
While the bone marrow may engraft within a few weeks, full immunological recovery can take many months, sometimes extending beyond a year, especially following an allogeneic bone marrow transplant. Because of this, patients must meticulously follow dietary restrictions and avoid large crowds and sick individuals. Furthermore, most patients require re-vaccination against common childhood diseases, since the conditioning regimen wiped out their previous immunity.
Addressing Late Effects and Survivorship
Survivors of BMT must be monitored for late effects, which are health problems that occur months or years after the procedure. These effects can include secondary cancers, thyroid dysfunction, cataracts, and infertility. Therefore, specialized survivorship clinics are often necessary. Because these patients have undergone such radical treatment, consistent, lifelong follow-up care is mandatory. Consequently, awareness of post-treatment options is just as important as the initial decision, similar to navigating options like fertility treatments abroad after cancer care.
🔗 Key Considerations for International Patients
For patients seeking a bone marrow transplant abroad, complex procedures necessitate careful planning. Firstly, securing treatment at an internationally accredited center is paramount. Moreover, this ensures that the facility adheres to the highest standards of care. Considering the long recovery time, patients and their caregivers must plan for an extended stay, often lasting 3 to 6 months, in the destination country. Indeed, travel logistics, pre-travel checklists, and specialized medical accommodation are critical elements to manage successfully.
The cost of BMT varies dramatically worldwide, making countries like Turkey an attractive option for high-quality, specialized care. When looking at options, patients should consider the expertise in specific transplant types, such as haploidentical BMT. Furthermore, the capacity of the center to manage post-transplant complications like GVHD is also a decisive factor. Because BMT is so resource-intensive, investigating the availability of support services, including psychological and nutritional counseling, is essential for a holistic recovery. Therefore, selecting a destination requires detailed due diligence.
Outbound Links for Credibility:
For a deeper understanding of the immunological basis of HLA matching, consult resources like those from major university medical centers that detail Human Leukocyte Antigen (HLA) Typing. Similarly, detailed reports on the latest advancements in conditioning regimens can be found in academic cancer journals, further explaining the complex balance between cancer eradication and toxicity, such as those that report on Reduced-Intensity Conditioning in BMT. Finally, comprehensive guidelines for survivorship care after BMT are often published by leading professional societies, which emphasize the management of late effects, similar to the guidelines for long-term health monitoring after complex procedures. This authoritative information helps to ground your understanding.
❓ Frequently Asked Questions (FAQ) about Bone Marrow Transplant
Below are answers to some of the most common and important questions concerning the bone marrow transplant procedure.
What is the primary difference between autologous and allogeneic bone marrow transplant?
The main distinction lies in the source of the hematopoietic stem cells. In an autologous bone marrow transplant, the patient receives their own stem cells. Conversely, in an allogeneic bone marrow transplant, the patient receives stem cells from a matched donor.
How long does the entire bone marrow transplant process take, from start to engraftment?
The complete process varies, but the critical phase—from the start of the conditioning regimen to initial engraftment (when the new stem cells begin producing blood cells)—typically takes between four to eight weeks, often requiring hospitalization for this entire period.
Is bone marrow transplant considered a cure for all types of cancer?
No, a bone marrow transplant is not a universal cure. It is primarily used for blood cancers like leukemia and lymphoma, as well as certain non-malignant disorders. Its success depends heavily on the specific disease, its stage, and the patient’s overall health.
What is the meaning of ‘conditioning regimen’ in a bone marrow transplant?
The conditioning regimen refers to the high-dose chemotherapy and/or radiation therapy administered to the patient immediately before the stem cell infusion. This vital step aims to eradicate any remaining cancer cells and suppress the patient’s immune system to prevent rejection of the new cells.
What is HLA matching, and why is it so important for an allogeneic bone marrow transplant?
HLA stands for Human Leukocyte Antigen. These are proteins found on most cells in your body. HLA matching determines how closely a donor’s tissue resembles the recipient’s. A close match is essential in an allogeneic bone marrow transplant to minimize the risk of Graft-versus-Host Disease (GVHD) and transplant rejection.
What is the most serious complication of an allogeneic bone marrow transplant?
Graft-versus-Host Disease (GVHD) is widely considered the most serious complication. This occurs when the transplanted immune cells recognize the recipient’s body as foreign and attack healthy tissues, most commonly the skin, liver, and gastrointestinal tract.
Can older patients receive a bone marrow transplant?
Age is less of a strict barrier today than in the past. While traditional BMT was limited, reduced-intensity conditioning regimens (also called ‘mini-transplants’) have made the procedure available to many older patients whose overall physical condition and organ function are strong.
How is a bone marrow donor’s stem cell collection performed?
Stem cells are usually collected through a process called apheresis. This involves the donor receiving injections of a growth factor to mobilize stem cells from the bone marrow into the peripheral blood. The blood is then filtered through a machine to collect the stem cells, similar to a platelet donation. Less commonly, cells are collected directly from the bone marrow under general anesthesia.
What does ‘engraftment’ mean during the recovery phase?
Engraftment is the crucial process where the transplanted stem cells settle in the recipient’s bone marrow and begin to multiply and produce new, healthy blood cells (red cells, white cells, and platelets). Engraftment is confirmed by monitoring blood cell counts. This biological process of cell differentiation is vital to many areas of medicine.
What kinds of non-cancerous diseases are treated with a bone marrow transplant?
Bone marrow transplants treat several non-malignant conditions. These often include severe aplastic anemia, sickle cell disease, thalassemia, and certain inherited immune deficiency disorders, effectively replacing the faulty blood-producing system. For those interested in the underlying genetic mechanisms, consider reading about preimplantation genetic testing.
Are there ethical considerations for receiving an allogeneic bone marrow transplant?
Yes, ethical considerations are vital, especially concerning donor consent, the psychological impact on both donor and recipient, and resource allocation. For instance, the use of cord blood or finding unrelated donors often involves complex legal and ethical frameworks. These ethical discussions also apply to areas like reproductive medicine.
How does a reduced-intensity conditioning (RIC) regimen differ from a myeloablative conditioning (MAC) regimen?
RIC uses lower doses of chemotherapy and/or radiation, which suppresses the patient’s immune system but does not completely destroy the bone marrow. In contrast, MAC uses very high doses designed to entirely eliminate all existing bone marrow cells. RIC is less toxic but relies heavily on the donor’s immune cells (GVL effect) to kill the cancer, whereas MAC aims to kill the cancer directly through the conditioning regimen.
What is the estimated recovery time for a bone marrow transplant?
Initial recovery (hospital stay and engraftment) takes about 4 to 8 weeks. However, the period of complete immune system recovery, particularly in allogeneic bone marrow transplant, is lengthy, often requiring 6 to 12 months for adults, and sometimes up to two years for children, before life returns to near-normal activities.
Why is a special diet required after a bone marrow transplant?
A special, low-microbial diet is essential during the early recovery phase when the patient is immunosuppressed. This diet minimizes the risk of consuming bacteria, fungi, or viruses that could cause a life-threatening infection. It typically involves avoiding raw fruits, vegetables, unpasteurized dairy, and uncooked foods until the immune system recovers.
1. /pgt-a-testing-process-accuracy-guide/
2. /kidney-donation-legal-countries-2025/
3. /car-t-therapy-pediatric-neuroblastoma-high-risk/
4. /medical-visa-definitive-patient-handbook/
5. /cardiac-surgery-eps-rfa-ablation-guide/
6. /health-checkup-2025-preventive-care/
7. /pre-travel-resources-checklists-patients/
8. /global-medical-treatment-regulations-guide/
9. /cheapest-country-cancer-treatment-2025/
10. /fertility-treatments-abroad-ivf-icsi-egg-donation-guide/
11. /best-country-open-heart-surgery-2025-guide/
12. /medical-travel-iran-2025-visa-guide/
13. /pgta-ivf-gender-selection-family-balancing-guide/
14. /preimplantation-genetic-testing-pgt-pgd-embryo-screening/
15. /fetal-gender-selection-ethics-guide/
16. /hair-transplant-understanding-your-long-term-results/
17. /aesthetic-surgeries-turkey-2025/Normal Outbound Links:
1. https://www.pennmedicine.org/for-patients-and-visitors/find-a-program-or-service/cancer-center/treatment-programs/bone-marrow-transplantation (University/Academic Source)
2. https://www.fredhutch.org/en/treatment/bone-marrow-stem-cell-transplant/what-is-bmt/hla-matching.html (Non-Competitor Research Center)
🌟 The Future of Bone Marrow Transplant
The field of bone marrow transplant is constantly evolving. Advances in haploidentical transplantation protocols have dramatically increased the number of available donors. Consequently, more patients now have access to this life-saving therapy. Additionally, cell-based therapies, which include TCR T-cell receptor therapy and targeted conditioning agents, promise to reduce toxicity while maintaining anti-cancer efficacy. For instance, new methods in cancer treatment leverage artificial intelligence to optimize patient selection and management, making BMT safer and more effective for a wider range of patients, including those with refractory blood disorders. It is a constantly moving frontier, providing hope where previously there was none.
Moreover, managing the emotional and psychological toll of a bone marrow transplant is also a crucial area of focus. Patients often deal with anxiety and depression related to the intensity of the treatment, the isolation period, and the risk of complications. Therefore, incorporating psychological support, similar to the counseling required for informed consent in fertility treatments, is a recognized standard of care. This holistic approach significantly improves long-term outcomes and quality of life for survivors.
When patients look internationally for this complex procedure, they often compare top-tier medical centers. For example, comparing specialized oncology centers is often as important as comparing general surgery options like kidney stone surgery in the best countries. The expertise of the hemato-oncology team is the single most important factor. Specialists rely on continuous research to refine their techniques, ensuring better graft function and lower toxicity rates. This dedication to cutting-edge science is what drives success in such high-stakes treatments.
In conclusion, the decision to proceed with a bone marrow transplant is monumental. It requires careful consideration of the risks, rewards, and the significant commitment to the prolonged recovery process. However, for many individuals facing life-threatening blood disorders, it represents the best and often only pathway to a definitive cure and a renewed lease on life. Wmedtour’s Oncology department provides support for patients navigating these difficult choices. General surgery options pale in comparison to the complexity of BMT.
Outbound Links (Normal):
For authoritative statistics on BMT outcomes and survival rates, please refer to the data published by the National Marrow Donor Program (NMDP). Additionally, comprehensive research on the long-term effects and quality of life for BMT survivors is available through academic research groups like the University of Texas MD Anderson Cancer Center.